When the pain came, I would scream the place down,” says John Sutherland as he remembers his worst days of physical agony. “I was on a hospital ward with lots of other people, and the feeling was just awful. Afterwards, when I came home, I’d lie on the couch and yell my head off. The pain would be constant until I was given morphine.”
Up until very recently John, who is 69 and lives in Inverness, had been in a very dark place. A former captain in the Queen’s Own Highlanders, his left leg had been amputated above the knee in 2003 after a lengthy battle with calf problems. He was able to put up with the stump and Phantom Limb pains for the next 13 years, until he hada five-point heart bypass operation in 2016.
“I honestly feel that the programme has saved my life. My wife tells everyone that she has her husband back.”
“I thought the operation would help my leg, but when the blood began flowing again the pain got much worse,” he says. “On a scale of one to 10, the pain that was with me 24 hours a day – what’s known as residual pain – went up to a six or seven, while the phantom pain – which is known sometimes as a spike or flare-up – was anywhere between seven and nine, and completely incapacitated me for hours on end. I would use a prescribed cocktail of opioid drugs which never hit the spot with my pain levels. It was horrendous!”
Fortunately for John, help was on hand. His Support Officer, Steve Burton, told himof a programme run at the King Edward VII’s Hospital’s Centre For Veterans’ Health in London. The Veterans’ Pain Management Programme, a 10-day residential course, wasset up in 2016 and is currently operating online because of coronavirus. It offers practical strategies to help improve quality of life alongside pain.


John was referred to the Centre – what did he have to lose? – and was invited onto the online programme in the height of lockdown in April. He was sceptical at first, but was hailing the programme’s therapists as “miracle workers” by the end of the course.
The programme leaves no stone unturned when it comes to helping those in pain, and includes reviewing medication, helping to understand pain better, and learning to control its day-to-day management.
The clinical team includes a consultant in pain medicine, a pain nurse, a psychologist, a physiotherapist, and a psychiatrist – all of whom are specialists in chronic pain and its management. Together, the psychologist, nurse and physiotherapist lead the programme and, crucially, sit in on every session, so they all learn the same things about the veterans and can jump in with the relevant advice when required.
INTEGRATED AND INTERDISCIPLINARY
“The programme is interdisciplinary, so myself, Claire [Fear, pain nurse] and Jannie [Van Der Merwe, psychologist] are all in every session at the same time,” explains physiotherapist Suzanne Brook. “It’s not just physio, then psychology, then nursing. It is integrated.”
At the start of the programme, the most important thing for the team to do is listen, says Suzanne. “It is vital for the veterans to feel as though they are being heard, and that we understand and acknowledge that the impact of living with pain is significant.
“Secondly, we want to show that the pain isn’t something they are imagining. Experiencing pain isn’t a case of needing to pull yourself together or toughen up, but it can be reduced. In a nutshell, we are looking at practical strategies to calm an over-sensitive central nervous system which will, in turn, allow people to feel more confident and in control.”
What those on the programme learn on Day One is crucial. “We carry out a session right at the start of the programme in whichwe look at the impact of persistent pain on the veterans’ lives, and it is massively significant,” says Claire Fear, the centre’s pain nurse. “The areas of their lives that are affected by their pain are far-reaching. Almost every aspect you can think of – from work to finances, relationships to mood, sleep, social life, exercise, fitness, hobbies... you name it, pain is right there in the middle. We talk about how our aim is to try to address all the ways in which chronic pain impacts on a person’s quality of life. Put simply, we are looking to improve the quality of the veteran’s life.”
THE BENEFITS CAN BE HUGE
For John, the programme was a revelation. “I was unsure how doing a course could help me get rid of my pain, but I soon realised that the idea is to understand the pain and then work through different stages, using the mind to understand the central nervous system,” he says.
“Everyone gets something different out of the programme but, for me, the most important thing I learned was mindfulness. You train the mind to identify unhelpful thoughts, break them down, and then reframe them. The technique freed me from depression and emotional distress... all the bits that went with the pain.
“We look at the impact of pain on the veterans' lives. The areas of their lives are affected are far-reaching"
“I apply the practices every day now, and through cognitive behavioural therapy and compassionate focused therapy, I’ve looked deep into my own mind. All this led to me being able to dwell less on distressingthoughts or images when in pain.”
The benefits for John have been huge. “My sleep pattern has changed. I sleep like a log now rather than spending half the night applying hot bean bags to my leg every 30 minutes, even though they weren’t actually achieving anything.
From being a nine or 10 every day, I’m not getting any great pain now. The programme is so good, it’s so different from sitting down with your GP who, it seems to me, is always on the clock.”
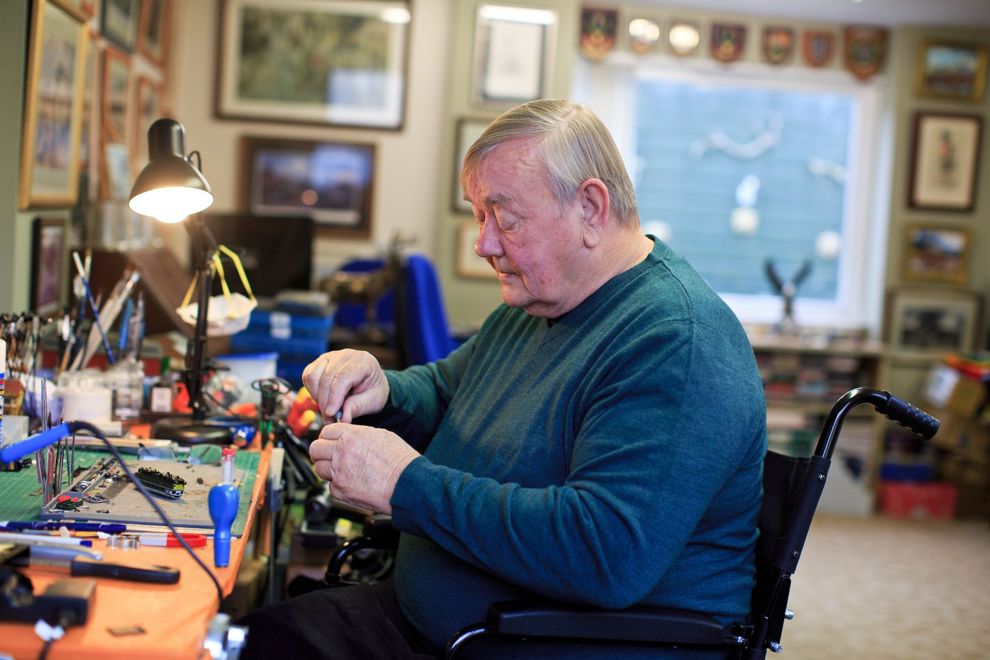

What is perhaps most incredible is that John is now almost completely medication free. “The programme made me realise that a lot of the medication I was on wasn’t helping at all. Claire helped me to reduce and finally stop taking the pills,” John says. “Medications are rarely, if at all, the complete answer. I have adopted a different solution, which has meant a monumental improvement in both my mental health and levels of pain. I also learned that exercise, no matter how bad you feel, is extremely important, and I do something every day. I would recommend the course to anyone in pain – you find out so much!”
NO TWO PEOPLE ARE THE SAME
The experts at the centre find themselves learning a great deal from their patients, too – and they believe veterans are always keen to learn. “They’re great to work with,” says Dr Jannie Van Der Merwe, the centre’s consultant clinical psychologist. “They are hungry for information, and we find we can present complex medical concepts to them at a high level, and they absorb them, take them on board, and really use them.


However, the team are quick to stress that no two people experience the course in the same way, and there can be no guarantee of success. “Because of the science of pain and how it is generated, we always point out that the programme’s primary aim isn’t the reduction of pain,” explains Suzanne. “It is about finding quality and meaning in what you do, day to day. And we don’t tell people exactly what to do, we guide them. This is often a huge relief for veterans, who often come from a boom-or-bust background.
“So, for example, I always look at specific strategies around movement and flexibility, with a view to helping the nervous system calm down rather than allowing it to be pushed. We go with a less-is-more approach, and we want to get veterans doing a bit of something they can repeat. It’s better than them doing something once and then never again.”
As the programme is run in groups, there’s also a hugely beneficial social aspect to the discussions. “We became a really tight group, all chatting on Zoom and staying in touch,” says John. “It’s great to be able to speak to people who really understand what you’ve been through. I honestly feel that the programme has saved my life. My wife tells everyone she meets that she has her husband back.”
To learn more, or to apply for a place on the Pain Management Programme, contact Caroline Dunne on 020 7467 4370 or at carolinedunne@kingedwardvii.co.uk
We can help
We are dedicated to assisting serving and ex-Service men and women who have suffered life-changing limb loss or the use of a limb, an eye or sight. We support these men and women in their communities throughout the UK. Click the link below to find out the different kinds of support we offer.
Get Support
Leave a comment
Join fellow Members and supporters to exchange information, advice and tips. Before commenting please read our terms of use for commenting on articles.